Phacoemulsification is a modern surgical technique used in cataract surgery. It is a minimally invasive procedure that involves the removal of the cloudy lens from the eye and the replacement with an artificial lens. This technique has revolutionized cataract surgery and has become the gold standard for treating cataracts. In this blog post, we will explore the procedure of phacoemulsification, the advanced techniques used, and the recovery process after the surgery.
Understanding Phacoemulsification
Phaco surgery involves the use of ultrasonic energy to break up the cloudy lens into tiny fragments, which are then gently suctioned out of the eye. This technique allows for a smaller incision size compared to traditional cataract surgery, resulting in faster healing and less postoperative discomfort.
The ultrasonic energy is delivered through a handheld device called a phacoemulsification probe. The probe emits high-frequency sound waves that create vibrations, causing the lens to break up into small pieces. The fragments are then aspirated out of the eye using suction. Phacoemulsification also offers the advantage of precise control during the surgery. The surgeon can adjust the power and speed of the ultrasonic energy to suit the specific characteristics of each patient’s cataract.
Why Is Phacoemulsification Done?
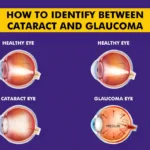
Phaco surgery is done to remove cataracts, which are caused by the clouding of the natural lens inside the eye. Cataracts can cause blurry vision, decreased color perception, and difficulty seeing at night or in low-light conditions.
By removing the cloudy lens and replacing it with an artificial lens, phacoemulsification can improve vision and restore clarity. This procedure is typically recommended when the cataract starts to significantly affect a person’s daily activities and quality of life.
Eligibility Criteria for Phaco Eye Surgery
Not everyone with cataracts is eligible for phacoemulsification surgery. The eligibility criteria may vary depending on the individual case and the surgeon’s recommendation. However, some common factors that determine eligibility include:
- Sufficient visual impairment due to cataracts
- Overall eye health
- Absence of other eye conditions or diseases that may affect the success of the surgery
- Realistic expectations and understanding of the potential risks and benefits
One must consult with an ophthalmologist to determine if phacoemulsification is the right option for you.
Phacoemulsification Surgery Mechanism
Phaco surgery is a cataract surgery technique using ultrasound to break up the lens. Components include:
Ultrasound (Phaco Handpiece): Emulsifies the cataract with high-frequency sound waves.
Aspiration (Suction): Removes emulsified lens material, maintaining a clear surgical field.
Irrigation: Provides a continuous saline flow to cool the handpiece, maintain eye shape, and flush out debris.
These components work together for efficient cataract removal, contributing to the surgery’s success and quicker recovery.
Phacoemulsification Surgery Procedure
The phaco surgery procedure involves the following steps:
- Preoperative assessment: The surgeon will evaluate your overall eye health and discuss the procedure with you. Several tests may be conducted to determine the appropriate power of the intraocular lens.
- Anesthesia: Local anesthesia in the form of eye drops or an injection will be administered to numb the eye and ensure a painless procedure.
- Incision: A small incision is made on the side of the cornea to access the lens.
- Capsulotomy: A circular hole is created in the front portion of the lens capsule, which holds the natural lens.
- Phacoemulsification: The phacoemulsification probe is inserted through the incision and used to break up the cataract into tiny pieces. The fragments are then suctioned out.
- IOL implantation: An artificial intraocular lens is inserted into the empty lens capsule to restore clear vision.
- Incision closure: The incision is self-sealing and usually does not require stitches.
- Postoperative care: The surgeon will provide instructions on postoperative care, including the use of eye drops and any necessary follow-up appointments.
Eye Issues Corrected by Phacoemulsification Surgery
Phaco eye operation corrects various eye issues associated with cataracts, including:
Blurred Vision: Removes the cloudy lens, restoring clear vision.
Glare and Halos: Reduces or eliminates visual disturbances, particularly at night.
Color Perception: Restores normal color vision by removing the opaque lens.
Presbyopia: Addresses age-related difficulty with near vision using multifocal or accommodating intraocular lenses.
Astigmatism: Corrects astigmatism with toric intraocular lenses during surgery.
Phacoemulsification Surgery Recovery: What to Expect
It is important to follow the surgeon’s instructions and attend all follow-up appointments for a smooth recovery.
- Rest and avoid strenuous activities on the day of surgery.
- Use of a protective eye shield, especially while sleeping.
- Mild irritation or foreign body sensation in the eye.
- Blurry vision initially, improving gradually.
- Medication adjustments based on recovery progress.
- Return to normal activities within a day or two.
- Gradual improvement in vision over several weeks.
- Rare events may include severe pain or sudden vision changes.
Advantages of Phacoemulsification Surgery
Phacoemulsion surgery surgery offers several advantages over traditional cataract surgery:
- Smaller incision size: Phaco eye operation requires a smaller incision, resulting in faster healing, and reduced risk of complications.
- Faster recovery: Phacoemulsification leads to a faster recovery compared to traditional surgery.
- Preciseness: The surgeon has control over the ultrasonic energy used in it, allowing for a tailored approach to each patient’s cataract.
Disadvantages of Phacoemulsification Surgery
- Cost: Phaco eye surgery can be more expensive than traditional cataract surgery due to the advanced technology involved.
- Potential complications: Although rare, phaco eye operation carries a small risk of complications, such as infection, bleeding, and damage to the surrounding structures.
It is important to discuss these cons with your surgeon to make an informed decision about the best treatment option for your cataract.
Risks and Complications Associated with Phacoemulsification Surgery
While phaco eye operation is considered a safe procedure, there are potential complications and risks associated with it. These may include rare risks of infection, swelling, retinal detachment, glaucoma, and dislocated intraocular lens. It is important to discuss these potential risks with your surgeon before undergoing phaco eye surgery.
Precautions to Take after Phaco cataract surgery
After phacoemulsification cataract surgery, it is important to follow certain precautions to ensure a smooth recovery and minimize the risk of complications:
- Use prescribed eye drops: Your surgeon will prescribe eye drops to prevent infection and inflammation. Follow the instructions for their usage carefully.
- Avoid rubbing or touching the operated eye: Rubbing or touching the eye can increase the risk of infection and delay healing.
- Protect your eye: Wear the protective shield provided by your surgeon, especially while sleeping, to prevent accidental injury to the eye.
- Avoid strenuous activities: Avoid activities that may strain or put pressure on the eyes, such as heavy lifting, bending, or vigorous exercise, for a few weeks after the surgery.
- Follow-up appointments: Attend all follow-up appointments with your surgeon to monitor your progress and ensure proper healing.
How Is Phacoemulsification Different from Traditional Cataract Surgery?
Phaco surgery differs from traditional cataract surgery in several ways:
Incision size: Phacoemulsification requires a smaller incision compared to traditional cataract surgery. This results in faster healing, less postoperative discomfort, and a reduced risk of complications.
Lens removal technique: The cloudy lens is broken up into small fragments using ultrasonic energy and then suctioned out. In traditional surgery, a larger incision is made, and the lens is removed in one piece.
Recovery time: Due to the smaller incision and less tissue disruption, phacoemulsification offers faster recovery time compared to traditional surgery.
Precision: Phaco surgery allows the surgeon to have precise control over the ultrasonic energy used, enabling a tailored approach to each patient’s cataract.
Cost: Phaco eye surgery can be more expensive than traditional cataract surgery due to the advanced technology involved.
FAQs
Which is better, phaco eye surgery or laser eye surgery for cataracts?
Phacoemulsification is the preferred surgical method for cataracts, while femto surgery is often used to further enhance accuracy and hasten recovery.
What is the difference between phacoemulsification and cataract surgery?
Phacoemulsion surgery is a modern cataract surgery technique that uses ultrasound to break up the lens, while “cataract surgery” is a broad term encompassing various methods, with phaco surgery being the most common.
What is the difference between phaco and mics cataract surgery?
Phacoemulsification (phaco) and microincisional cataract surgery (MICS) is the advanced version of phaco that involves smaller incisions (<2mm), potentially leading to quicker recovery.
Is Phaco surgery painful?
No, phacoemulsification surgery is typically not painful. Local anesthesia is used to numb the eye, and patients may feel pressure but not pain during the procedure.
What is the disadvantage of phaco?
Potential disadvantages may include rare complications like infection or inflammation.
Who is a good candidate for Phacoemulsification?
Most individuals with cataracts are suitable candidates for phacoemulsion surgery, but a thorough eye examination is needed to determine eligibility.
How long does a Phacoemulsification procedure typically take?
The surgery itself usually takes around 15 to 30 minutes, but overall time at the surgical center may be longer due to pre and postoperative processes.
How soon can I expect to see improvements in my vision after Phacoemulsification?
Vision improvement is often noticeable within a few hours after surgery, with optimal results achieved over several weeks.
Are there any restrictions on activities following Phacoemulsification?
Strenuous activities should be avoided initially, but most patients can resume normal daily activities within a day or two.
How long does it take to fully recover from Phacoemulsification?
Full recovery varies, but patients can generally expect a few weeks for complete healing and optimal visual results.
Can Phacoemulsification correct other vision problems besides cataracts?
Phacoemulsification primarily addresses cataracts; other vision issues may require additional interventions or procedures.