Retinal detachment is a serious eye condition that requires prompt attention. It occurs when the retina, the thin layer of tissue at the back of the eye, becomes detached from its normal position. This can lead to vision loss or blindness if not treated promptly. In this article, we will explore the retina detachment symptoms, emergency response measures, and the recovery process after undergoing surgery.
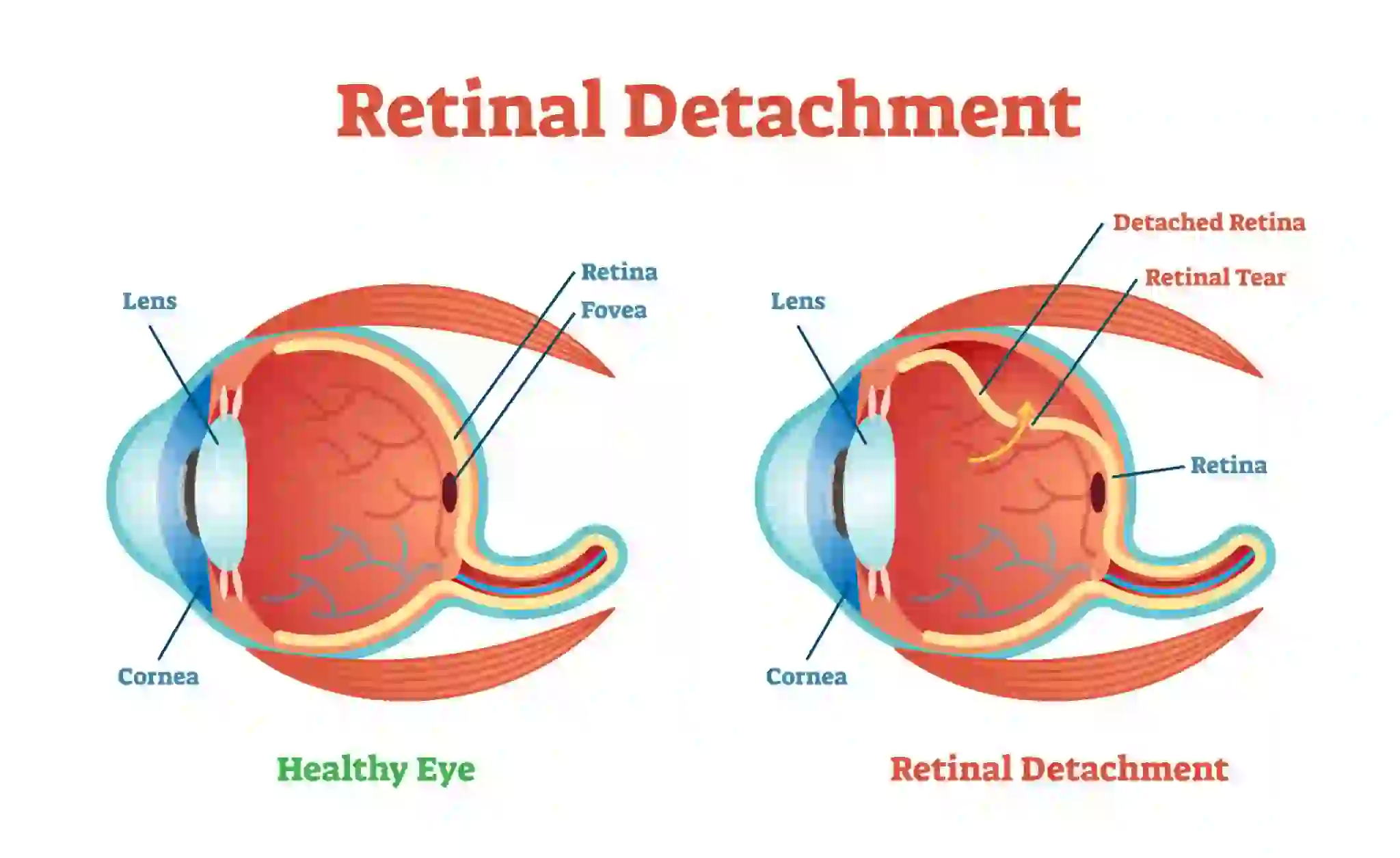
What Is Retinal Detachment?
Retinal detachment occurs when the retina, which is responsible for capturing and sending visual images to the brain, becomes separated from the underlying layers of the eye. This separation disrupts the normal functioning of the retina, leading to vision problems. There are three types of retinal detachment: rhegmatogenous, tractional, and exudative. Each type has different causes and risk factors.
Retinal detachment is a serious condition that requires immediate medical attention. If left untreated, it can lead to permanent vision loss. Understanding the signs and symptoms can help you identify the condition early and seek prompt detached retina treatment.
Signs and Symptoms of Retinal Detachment
Recognizing the retina detachment symptoms of retinal detachment is crucial for early diagnosis and treatment. While some people may experience sudden and noticeable changes in their vision, others may have more subtle symptoms. It is important to pay attention to any changes in your vision and seek immediate medical attention if you suspect retinal detachment. Some common signs and symptoms of retinal detachment include:
- Floaters: Seeing dark spots or specks that float across your field of vision.
- Flashing lights: Seeing flashes of light or sudden bursts of brightness.
- A curtain-like shadow: Experiencing a shadow or veil that obstructs part of your visual field.
- Blurred vision: Experiencing blurry or distorted vision, similar to looking through a foggy or wavy glass.
- Loss of peripheral vision: Noticing a decrease in your side or peripheral vision.
If you experience any of these symptoms, it is important to seek immediate medical attention. Remember, early diagnosis and detached retina treatment can greatly improve the chances of successful recovery.
Types of Retinal Detachment
There are three main types of retinal detachment: rhegmatogenous, tractional, and exudative. Each type has different causes and risk factors.
- Rhegmatogenous retinal detachment: This is the most common type and occurs when a tear or hole develops in the retina. As a result, fluid from the vitreous, the gel-like substance that fills the center of the eye, seeps through the tear and accumulates behind the retina, causing it to detach.
- Tractional retinal detachment: This type occurs when scar tissue on the surface of the retina contracts and pulls the retina away from the underlying layers. It is commonly seen in individuals with advanced diabetic retinopathy or other conditions that cause the growth of abnormal blood vessels on the retina.
- Exudative retinal detachment: Unlike the other types, exudative retinal detachment does not involve any tears or holes in the retina. Instead, it occurs when fluid accumulates behind the retina due to an underlying condition such as age-related macular degeneration, inflammatory disorders, or tumors.
Understanding the different types of retinal detachment can help in the diagnosis and treatment process. In the next section, we will explore the common causes of retinal detachment.
Causes of Retinal Detachment
Retinal detachment can occur due to various factors. Understanding the causes can help you identify potential risk factors and take preventive measures. Some common causes of retinal detachment include:
- Age: The risk of retinal detachment increases with age, especially after the age of 40.
- Eye trauma: Any injury to the eye, such as a direct blow or penetrating injury, can cause retinal detachment.
- Nearsightedness: People with severe nearsightedness (myopia) have a higher risk of developing retinal detachment.
- Previous eye surgery: Individuals who have undergone cataract surgery or other eye procedures may have an increased risk.
- Family history: Having a family history of retinal detachment increases the likelihood of developing the condition.
- Eye conditions and diseases: Certain eye conditions, such as lattice degeneration, retinoschisis, or uveitis, can increase the risk of retinal detachment.
It is important to note that not everyone with these risk factors will develop retinal detachment. However, it is essential to be aware of these factors and seek regular eye examinations to monitor your eye health.
Diagnosing Retinal Detachment
Diagnosing retinal detachment typically involves a comprehensive eye examination and various diagnostic tests. If you experience any symptoms or have risk factors for retinal detachment, it is important to seek medical attention promptly.
During the examination, an eye care professional will:
- Ask about your symptoms and medical history.
- Conduct a visual acuity test to assess your overall vision.
- Perform a dilated eye examination to examine the retina and other structures at the back of the eye.
- Use specialized tools, such as an ophthalmoscope or slit-lamp biomicroscope, to examine the retina in detail.
In some cases, additional tests may be recommended to confirm the diagnosis and determine the type and extent of retinal detachment. These tests may include ultrasound imaging, optical coherence tomography (OCT), or fluorescein angiography.
Emergency Response for Retinal Detachment: What to Do
Retinal detachment is considered a medical emergency that requires immediate attention. If you suspect retinal detachment based on the signs and symptoms you are experiencing, it is crucial to take the following steps:
Seek emergency medical care: Contact your eye doctor or visit the nearest emergency room as soon as possible. Time is of the essence in treating retinal detachment.
Avoid rubbing or applying pressure to the eye: Rubbing or applying pressure to the affected eye can worsen the condition and increase the risk of permanent vision loss.
Keep your head in an upright position: Positioning your head upright can help reduce the pressure on the retina and prevent further detachment.
Do not try to treat retinal detachment at home: Home remedies or over-the-counter treatments are not effective in treating retinal detachment. Only a medical professional can provide the necessary detached retina treatment.
Remember, early intervention is crucial for preserving your vision. Do not delay seeking medical attention if you suspect retinal detachment.
Treatment Options: Addressing Retinal Detachment
Treating retinal detachment typically involves surgical intervention to reattach the retina and prevent further vision loss. The specific treatment approach depends on the type, extent, and location of the detachment. Some common detached retina treatment options include:
Laser photocoagulation: This procedure uses a laser to seal the tears or holes in the retina, preventing fluid leakage and reattaching the retina.
Cryopexy: This technique uses extreme cold to freeze the retina around the tears or holes, creating scar tissue that seals the detachment.
Pneumatic retinopexy: In this procedure, a gas bubble is injected into the eye to push the detached retina back into place. Laser or cryopexy is then used to seal the tears or holes.
Scleral buckle surgery: This procedure involves placing a silicone band or buckle around the eye to push the wall of the eye closer to the detached retina, helping it reattach.
Vitrectomy: In many cases, a vitrectomy may be performed to remove the vitreous gel and replace it with a gas or silicone oil bubble. This helps to reattach the retina and restore vision.
The choice of treatment depends on various factors, including the type and severity of retinal detachment, the presence of other eye conditions, and individual patient factors. Your eye care professional will determine the most appropriate treatment plan for your specific situation. In the next section, we will discuss the recovery process after retinal detachment surgery.
Recovery After Retinal Detachment Surgery
After undergoing retinal detachment surgery, it is important to follow your doctor’s instructions for a smooth recovery and optimal outcomes. The recovery process may vary depending on the type and extent of the surgery performed. Here are some general guidelines for a successful recovery:
Take prescribed medications: Your doctor may prescribe eye drops or oral medications to prevent infection, reduce inflammation, and promote healing. It is important to take these medications as directed.
Avoid strenuous activities: During the initial stages of recovery, it is important to avoid activities that may strain the eyes or increase eye pressure. Your doctor will provide specific instructions on when you can resume normal activities.
Attend follow-up appointments: Regular follow-up appointments are crucial to monitor your progress and ensure proper healing. Your doctor will check the status of your retina and make any necessary adjustments to your treatment plan.
Protect your eyes: To prevent further injury or complications, it is important to protect your eyes from trauma, excessive sunlight, and other potential hazards. Wear protective eyewear as recommended by your doctor.
Avoid Air Travel: It’s crucial to avoid air travel for a period of time as advised by your surgeon. The changes in cabin pressure can potentially affect the healing of the retina and increase the risk of complications. Always follow your doctor’s guidelines regarding when it is safe to fly
The recovery timeline can vary from person to person, but most individuals experience significant improvement in vision within a few weeks to months after surgery.
How Can I Prevent Retinal Detachment?
While retinal detachment cannot always be prevented, there are certain measures you can take to reduce your risk:
Regular eye examinations: Routine eye exams are essential for detecting any early signs of retinal detachment or other eye conditions. Your eye care professional can identify risk factors and recommend appropriate preventive measures.
Protect your eyes from injury: Wear protective eyewear when engaging in activities that may pose a risk of eye injury, such as playing sports or working with tools or chemicals.
Manage underlying conditions: If you have any underlying conditions that increase the risk of retinal detachment, such as diabetes or high blood pressure, work closely with your healthcare provider to manage these conditions effectively.
Follow post-surgical instructions: If you have previously undergone eye surgery, such as cataract surgery, it is important to follow your doctor’s instructions for post-operative care and attend regular follow-up appointments.
Be aware of symptoms: Educate yourself about the signs and symptoms of retinal detachment, and seek immediate medical attention if you experience any changes in your vision.
While these preventive measures can reduce the risk of retinal detachment, it is important to remember that the condition can still occur despite taking precautions. Regular eye exams and early intervention remain crucial in preserving your vision.
Conclusion:
In conclusion, retinal detachment is a serious eye condition that requires prompt attention. Understanding the signs, emergency response measures, treatment options, and recovery process can help you make informed decisions and seek timely medical care. By taking preventive measures and staying vigilant about your eye health, you can reduce the risk of retinal detachment and protect your vision for years to come.
FAQs
Can one get a detached retina again after treatment?
Yes, it’s possible, especially if you’re at risk (e.g., nearsighted, previous detachment).
Is surgery always necessary for retinal detachment?
Yes, in most cases, surgery is needed to reattach the retina.
Are there any complications or risks associated with retinal detachment surgery?
Yes, risks include infection, bleeding, cataracts, and in rare cases, vision loss.
What is the long-term outlook for someone who has experienced retinal detachment?
With timely treatment, many regain useful vision, but long-term follow-up is crucial.
Is retinal detachment hereditary?
It can have genetic factors, but it’s mostly due to aging or trauma rather than direct heredity.