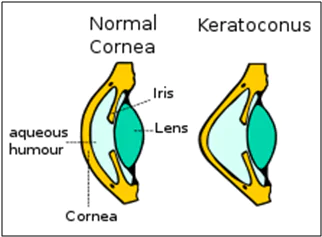
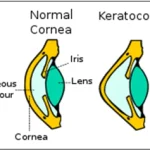
Keratoconus is an eye disorder which causes thinning of the cornea. It also causes a change in the shape of the cornea. The cornea of our eyes, which is a dome-shaped structure, turns conic under Keratoconus.Cornea is the outermost layer of our eyes. It allows the rays of light to enter the eyes and then, focuses the light rays on the retina for us to see. Thus, the impact of Keratoconus on our cornea leads to worse eyesight.
Many patients of Keratoconus find problems in carrying out some basic activities of day to day life. The simplest of things for a person with a normal cornea, such as reading, watching, driving, cooking, etc.becomes inconvenient for people suffering from Keratoconus.
Causes of Keratoconus
Keratoconus is an inherited condition that sometimes skips generations. Its onset is usually during puberty and is often related to allergies (hay fever, asthma and eczema). The cornea is a bit more elastic than normal and tends to alter in shape and thins out becoming cone shaped. Rubbing the eyes can aggravate the condition.
Symptoms of Keratoconus
The typical patient with undiagnosed keratoconus complains of deteriorating vision and frequent change in glasses. They may often report multiple images or ghosting of images and often relate a history of frequent refractive correction changes without much improvement in visual acuity. Patients may also report irritating symptoms such as intolerance to light (glare), photophobia and a recurrent foreign body sensation.
Diagnosis Tests for Keratoconus
A complete assessment for keratoconus includes:
- Refraction and visual acuity evaluation
- Intraocular pressure measurement
- Slit lamp examination and retina evaluation
- Corneal topography : Advanced topography systems such as the Pentacam and Orbscan assess the overall architecture of the cornea and help in early detection of keratoconus. These tests are also important in assessing the progression of keratoconus and in deciding the appropriate treatment options.
- Corneal Thickness measurement (Pachymetry)
KeratoconusTreatment Options
There are two aspects to keratoconus treatment – first we need to stop progression for which there is only one treatment namely, C3R or corneal crosslinking.Secondly, we look at the refractive error treatment and see if there is any aid to improve vision. These options include : spectacles, RGP contact lenses, special keratoconus contact lenses, INTACS (intracorneal ring segments) and ICL.
This decision as to what is best suited from the above choices for your eyes can only be taken after a complete assessment. Advanced cases with extreme thinning or scarring may not be amenable to treatment with these modalities. A corneal transplant is required in such cases.
- C3R/CXL – Corneal Collagen Cross linkingwith Riboflavin
Corneal collagen crosslinking, CXL or C3R is a relatively new form of therapy for keratoconus patients. This treatment is aimed at arresting the further progression of keratoconus by strengthening the corneal architecture.During the corneal crosslinking treatment, the superficial layer of the cornea (epithelium) is removed. Custom-made riboflavin drops saturate the cornea, which is then activated by ultraviolet light. This process has been shown in laboratory and clinical studies to increase the amount of collagen cross-linking in the cornea and strengthens the cornea.Collagen crosslinking is not a cure for keratoconus.
The aim of this treatment is to arrest progression of keratoconus, and thereby prevent further deterioration in vision and the need for corneal transplantation. Glasses or contact lenses will still be needed following the cross-linking treatment (although a change in the prescription may be required).
- What to expect after C3R/CXL?
After the procedure a bandage contact lens is applied. You may experience pain, lid swelling and foreign body sensation for 1-2 days after the procedure. The contact lens is removed 4-5 days after the epithelial healing is complete. Corneal haze develops in most cases following C3R/CXL. This resolves significantly over 3 weeks and completely over 6 months. The power of your glasses or fitting of contact lenses may change initially for few weeks following the procedure. The final prescription of glasses/ contact lenses is given 3-6 months following the procedure.
- INTACS
Intacs are thin plastic, semi-circular rings inserted into the middle layer of the cornea. The placement of Intacs remodels and reinforces the cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide improved vision. This can improve uncorrected vision, however, depending on the severity of the KC, glasses or contact lenses may still be needed for functional vision. The channels for placement of INTACs into the cornea can be created mechanically with a blade or with a precise femtosecond laser. The use of the femtosecond laser has greatly enhanced the safety of the procedure and improved surgical outcomes.Intacs procedure may be performed in conjunction with C3R for improved results.
- TORIC ICL
A collamer lens is implanted inside the eye to correct the refractive error completely or partially. A toric ICL may be performed in addition to the C3R procedure which aims to stabilize the refractive error.
- Corneal Transplant
In advanced stages – either a partial thickness (Deep Anterior Lamellar or DALK) or full thickness (Penetrating or PK) corneal graft may be required.In keratoconus, a corneal transplant is warranted when the cornea becomes dangerously thin or when sufficient visual acuity to meet the individual’s needs can no longer be achieved by glasses or contact lenses due to steepening of the cornea, scarring or contact lens intolerance.
Article: Understanding Keratoconus
Author: Dr Ritika | Feb 28 2017 | UPDATED 02:00 IST
*The views expressed here are solely those of the author in his private capacity and do not in any way represent the views of Centre for Sight.