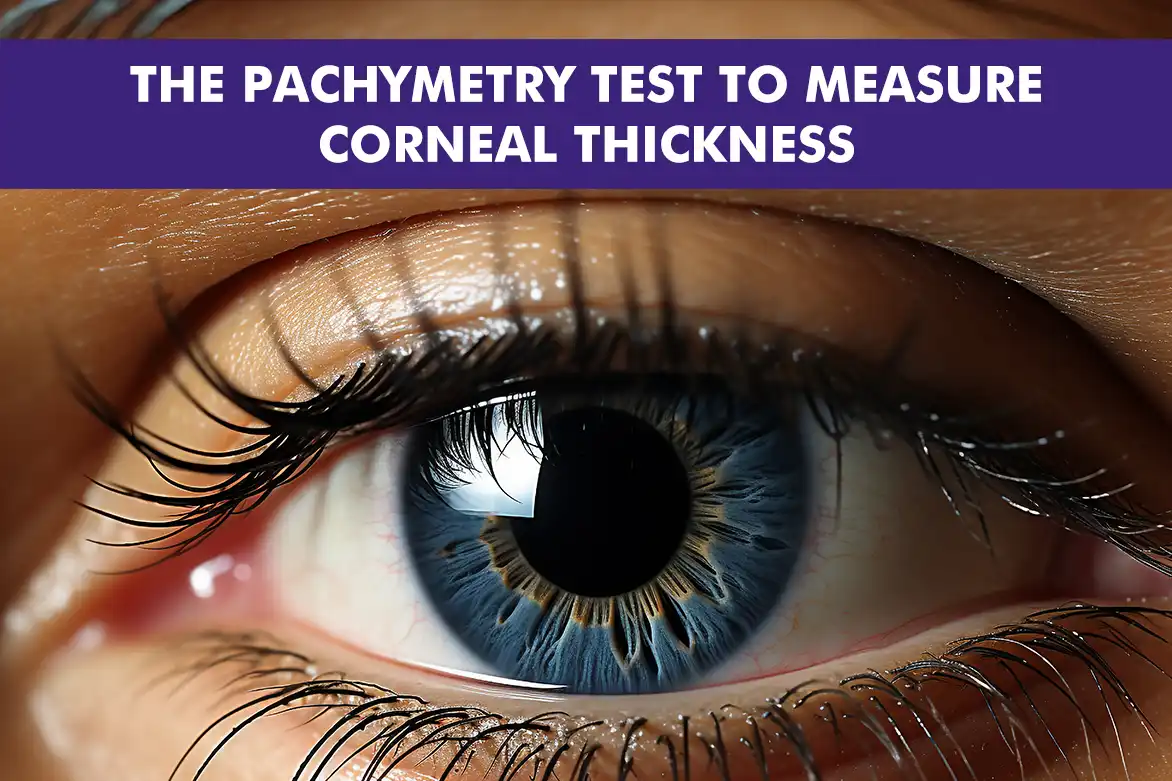
The pachymetry test is a crucial diagnostic tool in the field of ophthalmology. It measures the thickness of the cornea, the transparent front part of the eye that covers the iris and pupil. Accurate assessment of corneal thickness can help detect and manage various eye conditions.
In this article, we will delve into the details of the corneal pachymetry test, its importance, how it is performed, and the conditions it helps diagnose. We will also explore advancements in pachymetry technology and identify who might need this test.
Understanding the Pachymetry Test
The pachymetry test involves the use of specialized equipment to measure the thickness of the cornea. The test is non-invasive and quick, providing critical information about the cornea’s health.
There are three primary methods for performing pachymetry: ultrasound pachymetry, optical coherence tomography (OCT), and Scheimpflug imaging based (eg. Pentacam). Both methods are effective, though they use different technologies to achieve the same goal.
Why Corneal Thickness Matters
Corneal thickness is an essential parameter for a multitude of reasons, playing a crucial role in the diagnosis and management of various eye conditions. One of the primary conditions where corneal thickness is significant is glaucoma. In this case, increased intraocular pressure can signal a heightened risk of vision loss, and the thickness of the cornea can influence these pressure readings. Therefore, obtaining accurate measurements is vital for proper diagnosis and treatment. Additionally, corneal thickness is a critical consideration in refractive surgeries like LASIK. Surgeons rely on precise measurements to ensure the safety and effectiveness of the procedure, as it directly impacts surgical outcomes.
How the Pachymetry Test Is Performed
H3: Ultrasound Pachymetry:
- This method involves the use of a specialized probe that is gently placed on the surface of the cornea.
- The probe emits sound waves that travel through the corneal tissue.
- The time taken for these sound waves to bounce back to the probe is meticulously measured.
- This measurement provides an accurate assessment of the corneal thickness.
- The procedure is non-invasive and typically quick, making it a convenient option for both patients and practitioners.
- It is particularly useful in situations where precise corneal thickness measurements are required for diagnosing and managing eye conditions.
Optical Coherence Tomography (OCT):
- OCT employs advanced light wave technology to capture detailed cross-sectional images of the cornea.
- The patient is required to simply look into the OCT device, which is designed to be user-friendly and comfortable.
- As the patient gazes into the device, the light waves scan the cornea, creating high-resolution images.
- These images provide comprehensive data on the corneal structure and thickness.
- The procedure is swift and non-invasive, ensuring minimal discomfort for the patient.
- OCT is highly valued for its ability to deliver precise and detailed corneal measurements, aiding in the diagnosis and monitoring of various eye conditions.
Scheimpflug Imaging
- Devices based on Scheimflug imaging such as the Pentacam deploy high-resolution camera.
- It creates a 3D reconstruction of the cornea and its thickness profile.
- This is a preferred way of mapping corneal thickness prior to refractive surgery.
Understanding Average Corneal Thickness
The average corneal thickness in a healthy adult is generally found to be within the range of 520 to 550 micrometers. However, it is important to note that this measurement can vary significantly due to several influencing factors, including a person’s age, ethnicity, and any underlying health conditions they may have. Understanding what constitutes average corneal thickness is crucial for identifying potential abnormalities in the eye. For example, if a cornea is found to be significantly thinner than average, it may indicate the presence of a condition such as keratoconus. In keratoconus, the cornea progressively thins and begins to bulge outward, leading to vision problems.
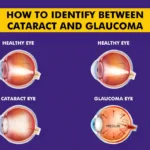
Conditions Diagnosed Through Pachymetry
Pachymetry is an essential diagnostic tool in the field of ophthalmology, as it allows for the diagnosis and monitoring of a variety of eye conditions. One of the primary conditions that can be assessed using pachymetry is glaucoma. In this case, accurate readings of intraocular pressure are vital for determining the risk and progression of the disease. Another condition that benefits from pachymetry is keratoconus, a disorder characterized by the thinning and distortion of the cornea. Furthermore, pachymetry is instrumental in evaluating corneal edema, which is the swelling of the cornea, and Fuchs’ dystrophy, a degenerative corneal disease. It also plays a significant role in both pre-operative and post-operative assessments for refractive surgeries, such as LASIK, ensuring that patients are suitable candidates and that the surgery has been successful. By providing precise measurements of corneal thickness, pachymetry aids in the effective management and treatment of these and other corneal diseases, ultimately contributing to better eye health outcomes.
Who Needs a Pachymetry Test?
Individuals who are at risk of developing glaucoma or have already been diagnosed with this eye condition are frequently advised to undergo the corneal pachymetry test. This recommendation is particularly pertinent for those who exhibit elevated intraocular pressure, as this can be a significant risk factor for glaucoma. Additionally, individuals with a family history of glaucoma are also considered prime candidates for this test, as genetic predispositions can increase the likelihood of developing the condition. Furthermore, patients who are contemplating undergoing refractive surgery, such as LASIK, will need to have this test performed to ascertain their suitability for the procedure. Moreover, individuals who exhibit symptoms or have conditions that affect the cornea may require pachymetry to ensure accurate diagnosis and effective monitoring of their eye health.
Advancements in Pachymetry Technology
Technological advancements have significantly improved pachymetry, enhancing its precision and efficiency as a diagnostic tool. Modern devices now offer cutting-edge technology for more accurate corneal thickness measurements, essential for diagnosing and managing eye conditions. These advancements result in quicker outcomes, enabling ophthalmologists to make timely decisions. Improved device designs also enhance patient comfort, reducing anxiety during testing.
Innovations like Scheimpflug imaging and advanced Optical Coherence Tomography (OCT) have revolutionized the field by providing detailed corneal images. Scheimpflug imaging uses a specialized camera for high-resolution images, allowing precise corneal mapping and early disease detection. Advanced OCT offers exceptional clarity and depth with light waves for cross-sectional images. These innovations lead to more accurate diagnoses and effective treatments, benefiting patients through early detection and intervention.
Conclusion
The pachymetry test is an indispensable tool in ophthalmology, offering valuable insights into corneal health. By measuring corneal thickness, it aids in diagnosing and managing various eye conditions, ensuring patients receive appropriate and timely care.
As technology continues to advance, the accuracy and ease of corneal pachymetry testing will only improve, further enhancing its role in eye health assessment and management.
FAQs
A pachymetry test measures the thickness of the cornea using ultrasound or optical technology.
Corneal thickness helps assess eye health, affecting diagnoses for conditions like glaucoma and suitability for refractive surgeries.
It’s typically done by placing a small probe or using optical scanning to measure corneal thickness quickly and accurately.
No, it’s painless and non-invasive, though you may feel slight pressure during the test.
Average corneal thickness ranges from 520 to 550 microns.
It depends on individual needs; people with glaucoma risks or planning refractive surgery may need regular testing, as recommended by an eye doctor.
Yes, it aids in glaucoma risk assessment by providing corneal thickness data, which affects eye pressure readings.