Cataract grading is an important process in assessing the severity of cataracts and determining the appropriate treatment options. It involves evaluating the cloudiness or opacity of the eye’s natural lens, which is affected by cataracts. By understanding cataract grading, patients and doctors can make informed decisions about the timing and type of treatment needed.
So, let’s explore the concept of cataract grading in detail, including its history, importance, and various grading systems used. We will also discuss the components involved in classification cataract and the techniques used to evaluate cataracts. Additionally, we will examine the cataract grading chart and what the different grades mean for vision.
What Is Cataract Grading?
Cataract grading refers to the process of evaluating the severity of cataracts in a patient’s eye. It involves assessing the cloudiness or opacity of the eye’s natural lens affected by cataracts. The grading helps determine the appropriate treatment options and the urgency of intervention.
Cataract grading takes into consideration various factors, such as the location of the cloudiness, extent of the cataract, as well as its impact on vision. The grading is typically done by an ophthalmologist using specialized tools and techniques.
History of Cataract Grading
The concept of cataract grading has evolved over time with advancements in medical understanding and technology. In the past, cataracts were simply described as being present or absent, without much consideration for their severity or impact on vision.
However, as medical knowledge and diagnostic tools improved, professionals recognized the need for a more comprehensive grading system. This led to the development of various cataract grading systems that provide a standardized approach to evaluating cataracts.
Why Is Cataract Grading Important?
Cataract grading chart is important for several reasons. Firstly, it helps determine the appropriate timing for cataract surgery. While cataracts generally progress slowly, they can significantly impair vision over time. Grading allows doctors to monitor the progression and recommend surgery when the cataracts start to significantly impact the patient’s quality of life.
Additionally, classification cataract provides valuable information for surgical planning. It helps the surgeon understand the complexity of the cataract and anticipate any potential challenges during the procedure. This allows for better preoperative planning and improves the chances of achieving optimal surgical outcomes.
How Is Cataract Grading Performed?
The process of cataract grading involves a comprehensive eye examination, including visual acuity tests, slit-lamp biomicroscopy, and dilated fundus examination. These examinations help assess the location, density, and impact of the cataract on vision. The doctor may also use additional imaging techniques, such as optical coherence tomography (OCT), to obtain detailed images of the cataract.
Types of Cataract Grading Systems
There are several different grading systems used to assess cataracts. These systems may vary in terms of the criteria used to evaluate cataracts and the grading scales employed. Some of the commonly used grading systems include the Lens Opacities Classification System (LOCS), the Oxford Clinical Cataract Classification and Grading System, and the Lens Opacity Case-Control Study (LOCS III) classification system.
Each grading system has its own advantages and limitations. The choice of grading system may depend on factors such as the purpose of evaluation, the preferences of the ophthalmologist, and the availability of resources.
Components of Cataract Grading
Creating a cataract grading chart involves the evaluation of various components of the cataract. These components include the location of the cataract within the lens, the density or opacity of the cataract, and the impact of the cataract on vision.
The location of the cataract can be classified as nuclear, cortical, or posterior subcapsular. The density or opacity of the cataract is typically graded on a scale, ranging from mild to severe. The impact on vision is assessed through visual acuity tests and other measurements of visual function.
By assessing these components, doctors can determine the severity of the cataract and make informed decisions about the appropriate treatment options.
Techniques for Cataract Grading
Cataract grading involves the use of various techniques to assess the severity of the cataract. These techniques include visual acuity tests, slit-lamp biomicroscopy, and dilated fundus examination.
Visual acuity tests measure the clarity of vision at different distances and help assess the impact of the cataract on vision. Slit-lamp biomicroscopy involves using a specialized microscope with a slit-shaped light beam to examine the different structures of the eye, including the lens. This allows the doctor to evaluate the location, density, and impact of the cataract.
Dilated fundus examination involves dilating the pupil and examining the back of the eye, including the lens. This provides additional information about the cataract and its impact on vision. Additional imaging techniques, such as optical coherence tomography (OCT), may also be used to obtain detailed images of the cataract.
Cataract Grading Chart
The cataract grading chart provides information about the different grades of cataracts and their impact on vision. The grades typically range from 1 to 4, with 1 being mild and 4 being severe.
In general, mild cataracts (grade 1) may cause minimal visual disturbances and may not require immediate surgical intervention. Moderate cataracts (grade 2) can cause noticeable visual impairments, such as blurred or hazy vision. Severe cataracts (grade 3) can significantly impact vision, making activities like reading or driving difficult. Very severe cataracts (grade 4) can cause near-total or total vision loss.
It is important to note that the grading chart is just one aspect of the overall evaluation, and the decision to undergo cataract surgery is based on a combination of factors, including the patient’s symptoms, visual needs, and overall health.
Challenges and Limitations of Cataract Grading
Although cataract grading is a valuable tool in assessing cataracts, it has certain challenges and limitations. One challenge is the subjective nature of grading, as it relies on the interpretation of the examiner. Different examiners may have variations in their assessment, leading to inconsistencies in grading.
Another limitation is that cataract grading does not capture the full spectrum of visual symptoms experienced by patients. Some individuals may have significant visual disturbances even with mild cataracts, while others may have minimal symptoms despite severe cataracts.
Furthermore, cataract grading may not fully account for other factors that can impact vision, such as the presence of other eye conditions or the individual’s visual demands. It is important for doctors to consider these factors in conjunction with the grading results when making treatment decisions.
Applications of Cataract Grading in Cataract Surgery
Cataract grading plays a crucial role in cataract surgery. It helps the surgeon assess the complexity of the cataract and plan the surgical approach accordingly. For example, a more advanced cataract may require specialized techniques or equipment during surgery.
Additionally, cataract grading allows the surgeon to set appropriate expectations for the patient regarding the potential visual outcomes of the surgery. By understanding the severity of the cataract, the surgeon can provide realistic expectations and discuss the potential need for additional procedures, such as the implantation of an intraocular lens (IOL). Overall, cataract grading enhances the precision and effectiveness of cataract surgery, leading to improved visual outcomes for patients
Know more about types of Intraocular lenses
FAQs
What are the grades of cataracts?
Cataracts are typically graded on a scale from 1 to 4, with 1 being early-stage and 4 being advanced.
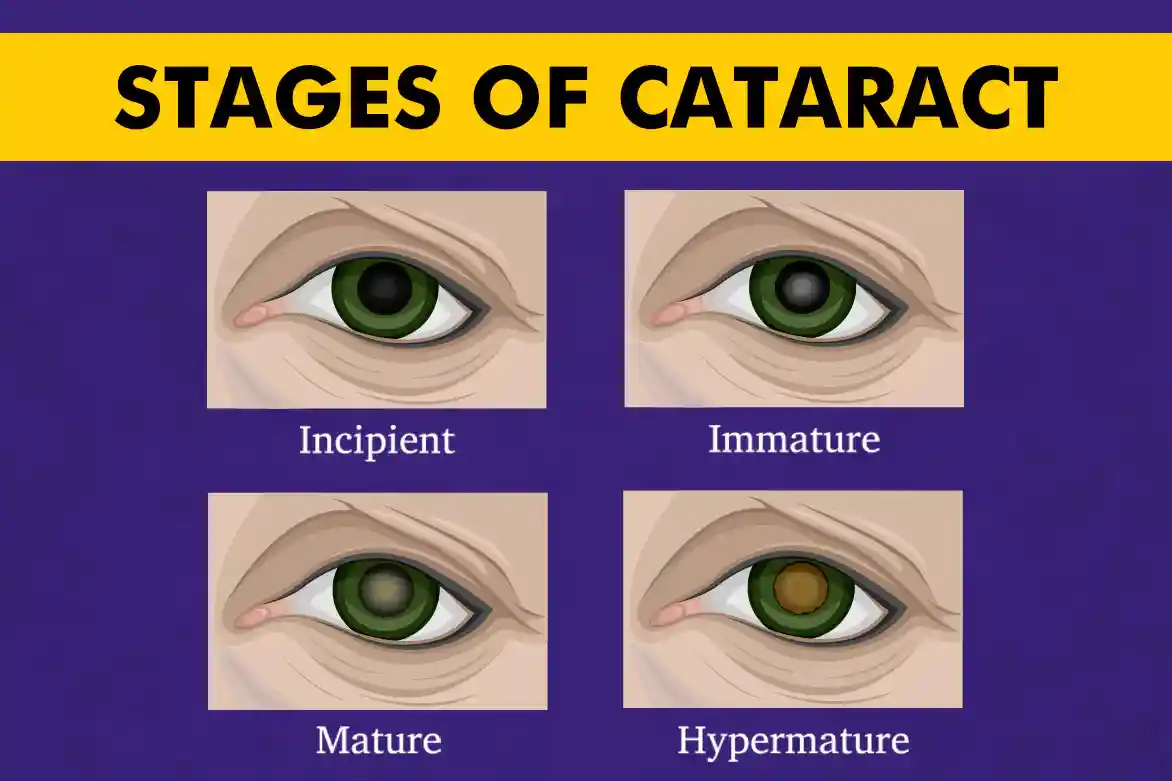
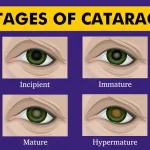
What are the 4 stages of cataract?
The stages are:
Stage 1: Early, minimal clouding of the lens.
Stage 2: Mild, noticeable clouding affecting vision slightly.
Stage 3: Moderate, significant clouding leading to vision impairment.
Stage 4: Severe, advanced clouding causing significant vision loss.
What is a Grade 4 cataract?
Grade 4 cataract refers to the most severe stage where the clouding of the lens is advanced, causing significant vision loss.
What is stage 3 cataract?
Stage 3 cataract is characterized by moderate clouding of the lens, resulting in significant vision impairment.
What is cataract grading?
Cataract grading involves assessing the severity of cataracts based on factors such as cloudiness, vision impairment, and impact on daily activities.
What is the classification of cataracts?
Based on cataract grading chart, cataracts can be classified based on location (nuclear, cortical, posterior subcapsular) or by cause (age-related, congenital, secondary).
What is cataract grade 8?
Cataract grading typically ranges from 1 to 4; there’s no standardized Grade 8. Higher grades generally indicate more severe cataracts.
What factors are considered in cataract grading?
Factors include degree of cloudiness, visual acuity, impact on daily activities, and patient symptoms.
Read blog on Symptoms of Cataract
Also know about Visual Acuity Test
How does cataract grading influence treatment decisions?
Cataract grading helps determine the urgency and type of treatment needed, whether it’s through lifestyle adjustments, prescription glasses, or surgical intervention. Higher grades of cataract (grade 4) offer greater complexity in surgery.
Can cataract grading be done remotely or virtually?
Yes, cataract grading can be done remotely through telemedicine platforms by evaluating patient-reported symptoms and images.
How does cataract grading differ from cataract diagnosis?
Cataract grading assesses the severity and impact of cataracts, while diagnosis involves identifying the presence of cataracts through clinical examination and testing.