If you have been diagnosed with diabetes, make sure you visit the eye doctor regularly. People with diabetes are at a higher risk of peripheral neuropathy and various eye complications. High blood sugar is a leading cause of glaucoma, cataract and diabetes retinopathy. According to the National Health Portal of India (NHP India), one of the leading causes of chronic blindness includes diabetic retinopathy. Although diabetic patients are indeed at a higher risk of blindness than people without diabetes, however, diabetic people can also have healthy eyes given that they consult an eye specialist regularly, properly take care of their diet and medications and adopt good lifestyle practices.
What is Diabetic Retinopathy?
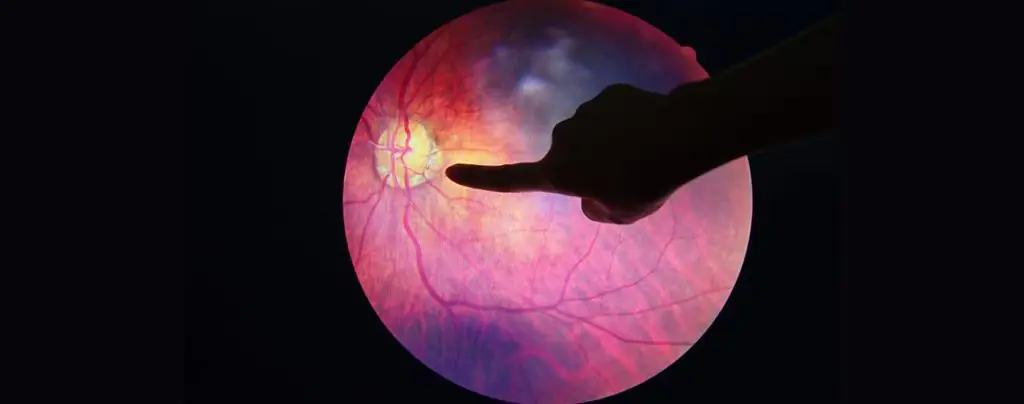
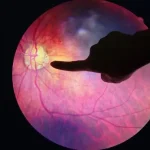
Diabetic retinopathy is a diabetes complication that damages nerves and blood vessels of the light-sensitive tissues at the back of the eye known as the retina. The purpose of retina is to convert the light into neural signals and send them back to the brain for visual recognition. The high blood sugar levels can restrict the movement of blood in the retina, causing the blood vessels to swell and leak. In some of the rare cases, new blood vessels can grow on the retina abnormally. If not treated on time, this may lead to loss of vision in the long run.
Diabetic Retinopathy Symptoms
During the early stages, a person having this condition may not even know it.As it starts getting worse, symptoms will begin to arise such as: · Seeing lots of floaters (various shapes that appear to be floating in the field of vision) · Having blurred vision · Inconsistent focus · Colour blindness · Poor vision especially at night · Loss of vision
Stages
Diabetic Retinopathy may progress through four stages:- Stage 1) Mild Nonproliferative Diabetic Retinopathy (NPDR): This type of retinopathy is indicated by the existence of microaneurysms (small swellings that leak fluid into the retina). Structural changes in the retina are caused due to mild NPDR as an anatomical effect of diabetes. Stage 2) Moderate Nonproliferative Diabetic Retinopathy: At this stage, blood vessels swell up that hinders the free flow of blood to the retina, they may also become totally incapable of transferring blood, ultimately leading to Diabetic Macular Edema (DME), a condition wherein fluid gets accumulated in the macula-part of the retina that controls the detailed vision. Stage 3) Severe Nonproliferative Diabetic Retinopathy: As the disease progresses, many more blood vessels are blocked, cutting down the already deprived blood supply to the retina. In the areas of retina where this blockage happens as a reaction, the retina starts developing new blood vessels that tend to be fragile and abnormal. Stage 4) Proliferative Diabetic Retinopathy (PDR): At this advanced stage, due to full blood vessels blockage and release of growth factors, new abnormal and fragile blood vessels develop on the inside surface of the retina and into the vitreous gel (clear fluid in the center of the eye). The scar tissues can shrink and may lead to retinal detachment-pulling away the retina from the tissue underneath that can cause permanent loss of vision.
Diabetic Retinopathy Treatment
The diabetic retinopathy treatment includes: · Laser treatment: It is used to treat the growth of abnormal blood vessels that develop in the retina and also treat the Diabetic Macular Edema(DME). · Eye injections: They are used to avoid the formation of new blood vessels in the retina. · Eye surgery: In the case of advanced retinopathy, when laser treatment is not possible, an operation known as Vitreoretinal surgery is carried out to remove the extra quantity of blood and scar tissues that have been accumulated in the eye.
Prevention
People with diabetes (Type 1 or Type 2) are at the risk of diabetic retinopathy when blood glucose levels are not controlled adequately. The longer this state exists, the higher are the chances of this disease. Pregnant women with gestational diabetes face a higher risk. Smoking, high blood pressure and high cholesterol level also increase the risk of diabetic retinopathy. It’s not always possible to prevent this disease, however, it’s possible to keep severe complications at bay by exercising the following: ·Manage your diabetes: Apart from being punctual to your diabetes medications, make sure you also adopt a healthy lifestyle. Make exercise and a healthy diet a part of your daily routine. Also, do monitor your blood sugar level regularly, and consult your doctor about its frequency. ·Consult your doctor about glycosylated hemoglobin test: The glycosylated test (also called hemoglobin A1c test) provides an average blood sugar level over the past 2 to 3 months period to make treatment adjustments. ·Manage your cholesterol and blood pressure: Adopting a healthy lifestyle and managing weight is necessary. Also, consult your doctor at regular intervals. ·Quit smoking: Smoking is a key catalyst for various diabetes-related health problems. In any case, it’s always suggested to avoid smoking.
A Word from CFS
The biggest challenge with diabetic retinopathy is that it remains undiscovered until it reaches the advanced stage. It’s also not possible to experience the damage it has caused to one’s eyes until a doctor discovers it during the regular eye check-up. Having a good lifestyle that includes doing regular exercise along with a balanced diet, getting timely check-ups and taking medications or insulin prescribed by your doctor are some of the steps you must follow strictly. If you notice any changes in vision, see your eye doctor on a priority basis.